Presentation:
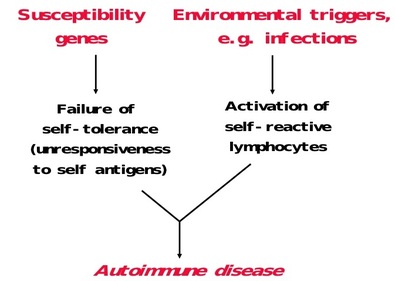
Pathogenesis:
- Genetic susceptibility to developing autoimmune hepatitis has been associated with the HLA haplotypes B8, B14, DR3, DR4, and Dw3
- C4A gene deletions are associated with the development of autoimmune hepatitis
- Viruses:
- Drugs
Investigations:
- CBC (pancytopenia secondary to hyperspleenism)
- Bilirubin, ALT, AST, ALP (usually all raised)
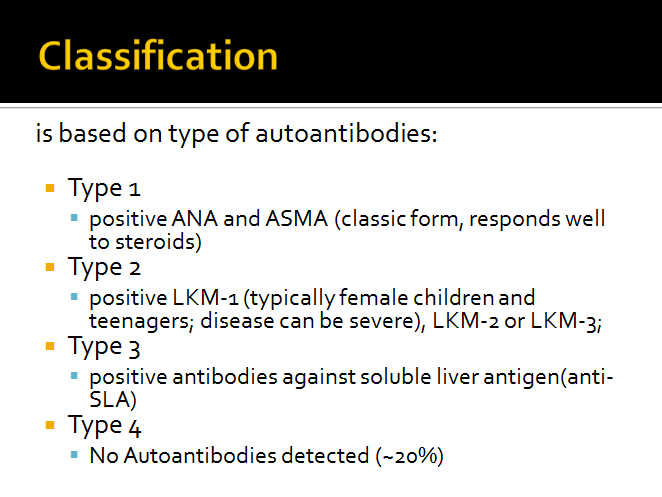
- Autoantibodies
- ANA
- ASMA
- Anti-LKM
- Anti – SLA
- Serum IGg Levels
- Liver Biopsy
- Investigations to rule out other causes of CLD
- AntiHCV, HBsAg
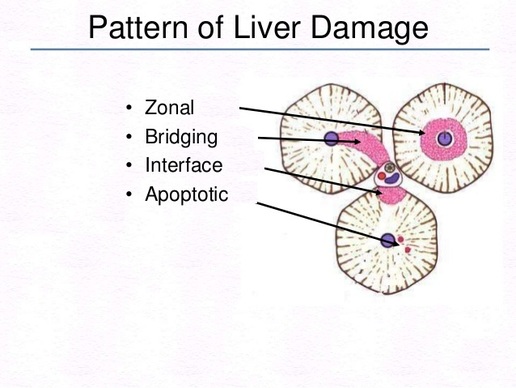
Liver Biopsy
It refers specifically to a loss and degeneration of (limiting plate) hepatocytes at the lobular-portal-interface, producing a moth-eaten irregular appearance.
- In Autoimmune Hepatitis Bridging or interface hepatitis occurs
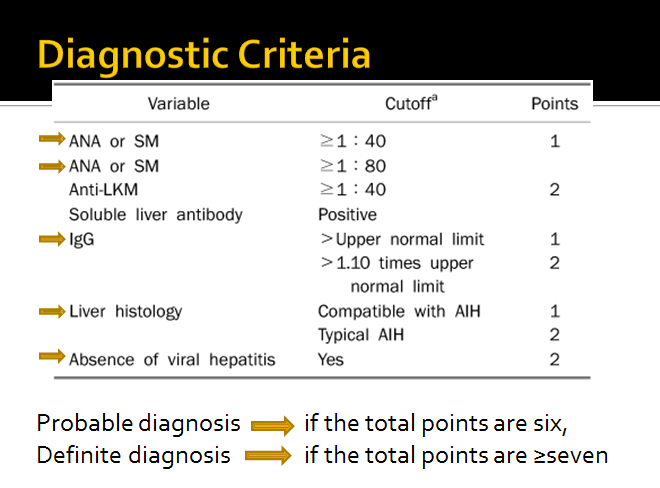
How to Diagnose:
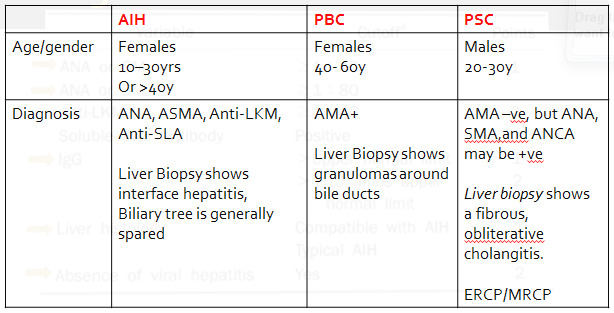
Differential Diagnosis
- Primary Biliary Cirhosis
- Primary Sclerosing Cholangitis
- Chronic Viral Hepatitis
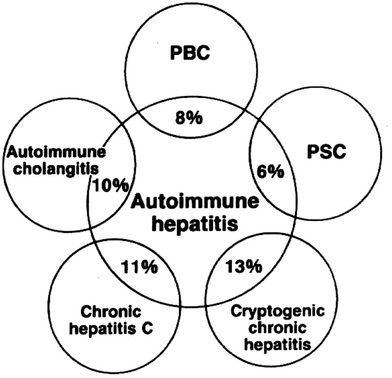
- Overlap Syndrome
- AIH plus PBC, AIH plus PSC
Overlap Syndromes:
Associated Conditions
- Type I diabetes mellitus
- Thyroiditis
- Idiopathic thrombocytopenic purpura
- Ulcerative colitis
- Rheumatoid arthritis
- Primary biliary cirrhosis and primary sclerosing cholangitis occasionally overlap with AIH
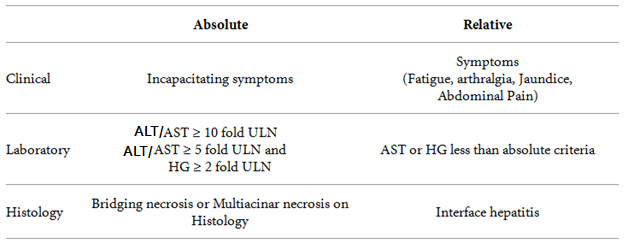
Indications for treatment
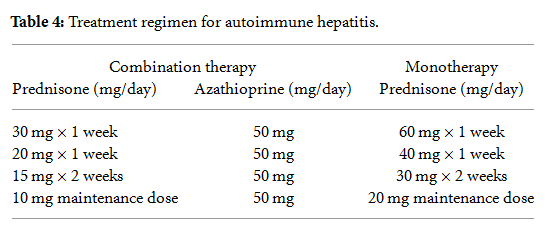
Treatment
First Line Drugs:
- Prednisolone
- Azathioprine
- Cyclosporine
- Tacrolimus
- Mycophenolate Mofetil
Liver transplantation
- Osteoporosis, Diabetes, HTN, Obesity, Acne, Depression
- Cytopenias
- Pregnancy
Second Line drugs are considered if there is no improvement in clinical, lab and histological features after 6 weeks of therapy
Endpoints of treatment
- Normalization of ALT
Secondary End Point
- Normalization of Histologic activity
Final Goal
- To achieve sustained remission without need of drug therapy or at lowest dose possible, and maintaining the hepatic reserve

 RSS Feed
RSS Feed